SENIOR doctors have demanded “immediate” government action to tackle the disproportionate number of deaths among ethnic minority communities suffering from the Covid-19 virus.
Although the government announced on April 16 that it would launch an inquiry into why people from black, Asian and minority ethnic (BAME) backgrounds appear to be disproportionately affected by coronavirus, there have been no details about which factors would be investigated and when the report would be submitted.
The call from doctors comes after weeks of reports of increasing cases of BAME patients dying of coronavirus in the UK.
According to the Mail on Sunday, 25 of the 26 doctors and two-thirds of NHS staff who have died from the coronavirus are from ethnic minority groups. Previously, it was revealed that a third of those in intensive care were from BAME backgrounds.
Dr Chaand Nagpaul, chair of the British Medical Association (BMA), told Eastern Eye that “immediate steps” needed to be taken to protect higher-risk BAME doctors and key workers.
“Until we can develop a detailed understanding of the threats they face, steps must be put in place to protect our BAME communities now,” he said.
“This could include those at greatest risk, including older and retired doctors, [healthcare staff] not working in potentially infectious settings as well as being given all necessary protective equipment.”
Dr Chandra Kanneganti, chairman of the British International Doctors Association, was quoted as saying by the Mail on Sunday that asking BAME NHS staff to continue working on the frontline was “like asking them to commit suicide”.
He has also urged the government to set up a task force to look into the issue.
“It needs to happen in the next few days, not weeks or months,” the GP said. “Without doctors from black, Asian and ethnic minority groups, the NHS would have collapsed by now due to the Covid-19 crisis.
“Yet asking them to carry on serving on the front line when some may be at increased risk of infection is like asking them to commit suicide.”
According to a BMA survey published last Friday (24), BAME doctors claim to have been disproportionately affected by the chronic shortages of personal protective equipment (PPE) across the NHS. Analysis by the BMA found that 64 per cent of BAME doctors surveyed said they felt “pressured” to work in settings with inadequate PPE, compared to 33 per cent of doctors who identified as white.
Dr Nagpaul has previously said that BAME doctors suffered bullying and would not speak out if adequate PPE was not available.
A junior BAME doctor described themselves as being “stressed out, concerned and afraid” of contracting the virus.
“My colleagues are getting the infection one after another and going off sick, it won’t be too long for me to get it. Hopefully, it won’t be that bad or cost me my life.”
Another described unsafe “donning and doffing” techniques while wearing PPE.
“BAME doctors are dying from coronavirus in the line of duty. Most of them have underlying medical conditions. They are not being risk assessed nor tested.”
In a letter to NHS England chief executive Simon Stevens, Dr Nagpaul said: “We... need to ensure there is sufficient supply of effective PPE to meet different needs.
“Some medics, such as Sikh and Muslim doctors, wear beards for religious reasons and we have heard they are facing difficulties in getting alternative respirators like PAPR [powered, air-purifying respirator] hoods when filtering facepiece 3 [FFP3] masks cannot be fitted.”
“These doctors have [often] come from other parts of the world to provide vital care in our health service, and they have sadly paid the ultimate price,” Dr Nagpaul said last week.
Parliamentary figures published last July showed that some 153,000 workers out of 1.2 million NHS staff were non-British.
Around 52,000 staff were Asian nationals, according to data.
Among the most common 16 nationalities of people working for the NHS were Indian (21,207), Nigerians (6,770) and Zimbabweans (4,049).
Labour MP Dr Rosena Allin-Khan has also spoken of the risks that ethnic minority NHS employees are taking and urged for them to be protected.
Dr Allin-Khan, who has been working shifts at London’s St George’s Hospital in her Tooting constituency, told Eastern Eye:
“Disproportionately, so many of the frontline staff who have died are from BAME communities. Every day they put themselves in harm’s way to save and support the lives of others. We must do everything to protect them, their families and communities who have been hit hardest by the virus – not at some point in the future, but right now.”
The chairman of the NHS Confederation, Lord Victor Adebowale, has also urged the government to agree on a deadline for the impending review. Noting that ethnicity was not currently recorded on death certificates, the peer has warned that the initial figures on BAME patients could “be the tip of the iceberg”.
“This is a matter of life or death for frontline staff from BME communities and needs urgent focus,” he said. “It is vital that we identify the factors behind these deaths and what can be done both now and in future to mitigate risks.”
On the government inquiry, Dr Nagpaul called for appropriate real-time data to understand why and how the virus appeared to have such a disproportionate toll on BAME communities and healthcare workers.
He has urged daily updates not just on ethnicity but also on protected characteristics of all patients in hospital as well as levels of illness in the community, which is not currently recorded.
“Since April 17, data on the ethnicity of those who have died has been collected, but we need more data around who these people are, including their age,” he said.
Dr Nagpaul has also suggested that data be collected on the deaths of frontline workers, to develop a better understanding of how people’s job roles and lives may be putting them further at risk.
In response to Eastern Eye, Public Health England (PHE) could not confirm any further details on the government investigation on BAME groups.
Dr Nagpaul added that public health messaging on social distancing and measures to prevent infection needs to be more tailored to reflect the lives and circumstances of BAME people. He expressed concern that the lack of appropriate messaging, combined with language barriers, could meant that guidance may not be reaching communities as it should.
“PHE has made none of its Covid-19 campaign resources on their website available in languages other than English,” he noted. “When you look at the coronavirus “hotspots” – London and the West Midlands – these are areas where there are the largest proportion of people who do not speak English well, and therefore language is a crucial factor.”
The Welsh government has also taken steps to address the disproportionate number of deaths in the BAME community.
Professor Keshav Singhal, the chair of British Association of Physicians of Indian Origin (BAPIO) in Wales, and BAPIO secretary Dr Hasmukh Shah are two of the doctors advising the Welsh government on the issue. They now speak with officials once a week on a Skype conference call.
Last week, Professor Singhal and Dr Shah wrote to NHS England & Wales about the Covid-19-related high mortality rates among the BAME population and their concerns about the high death rate.
“I’m hoping we can help the Welsh government so that we can make sure there are steps taken to address the high mortality rate in BAME groups,” Dr Shah told Eastern Eye.
Meanwhile, some NHS staff have begun legal proceedings against the government on the lack of PPE available to frontline workers.
NHS doctors Dr Nishant Joshi and his pregnant wife, Dr Meenal Viz, launched legal action last week as they alleged shortage of PPE across the NHS during the Covid-19 crisis.
In addition to NHS staff, concerns have also been raised about the safety of other key workers who do not have sufficient protection from the virus. Roles such as taxi drivers, bus drivers, or supermarket workers are more likely to be filled by people from ethnic minority groups.
It was reported last week that six minicab drivers had died from symptoms linked to Covid-19. Zahid Pervaiz, 65, was the latest to die after reportedly picking up a passenger with the virus, it was reported last Thursday (26).
London mayor Sadiq Khan confirmed last month that more than 20 London transport workers had died after contracting the virus. More than a quarter of workers in London operating Tube trains and buses are from ethnic minority backgrounds.





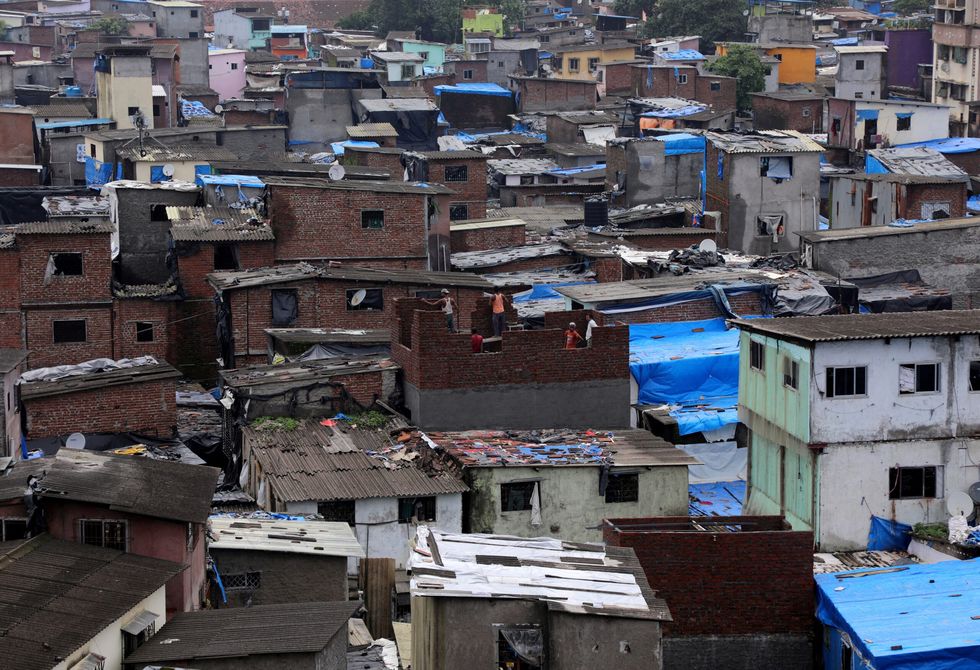 Dharavi slum in Mumbai
Dharavi slum in Mumbai













During the hearing, Clifford denied all the charges except for the rape charge, which was added to the indictment at the session. (Photo: Hertfordshire Police /Handout via REUTERS)
Man pleads not guilty to murder of BBC presenter's family
A 26-year-old man has pleaded not guilty to charges of murdering the wife and two daughters of BBC sports commentator John Hunt in a crossbow and knife attack.
Kyle Clifford, who also faces charges of rape, appeared via video link at Cambridge Crown Court on Thursday.
Clifford, arrested in July after a manhunt, is charged with three counts of murder, one count each of rape and false imprisonment, and two counts of possessing offensive weapons – a 10-inch knife and a crossbow.
During the hearing, Clifford denied all the charges except for the rape charge, which was added to the indictment at the session.
He is expected to enter a plea for that charge at a later date.
The victims were Carol Hunt, 61, wife of horseracing commentator John Hunt, and their daughters Louise, 25, and Hannah, 28.
An earlier hearing revealed that Louise had been found tied up and that both she and her sister had been shot with a crossbow, while their mother had been stabbed with a knife.
The fatal attack occurred at the family’s home in Bushey, a commuter town near Watford, northwest of London.
(With inputs from AFP)