A CONTROVERSIAL NHS data sharing plan has been backed by leading doctors and experts, but they have called for transparency over what is being gathered and for what purpose.
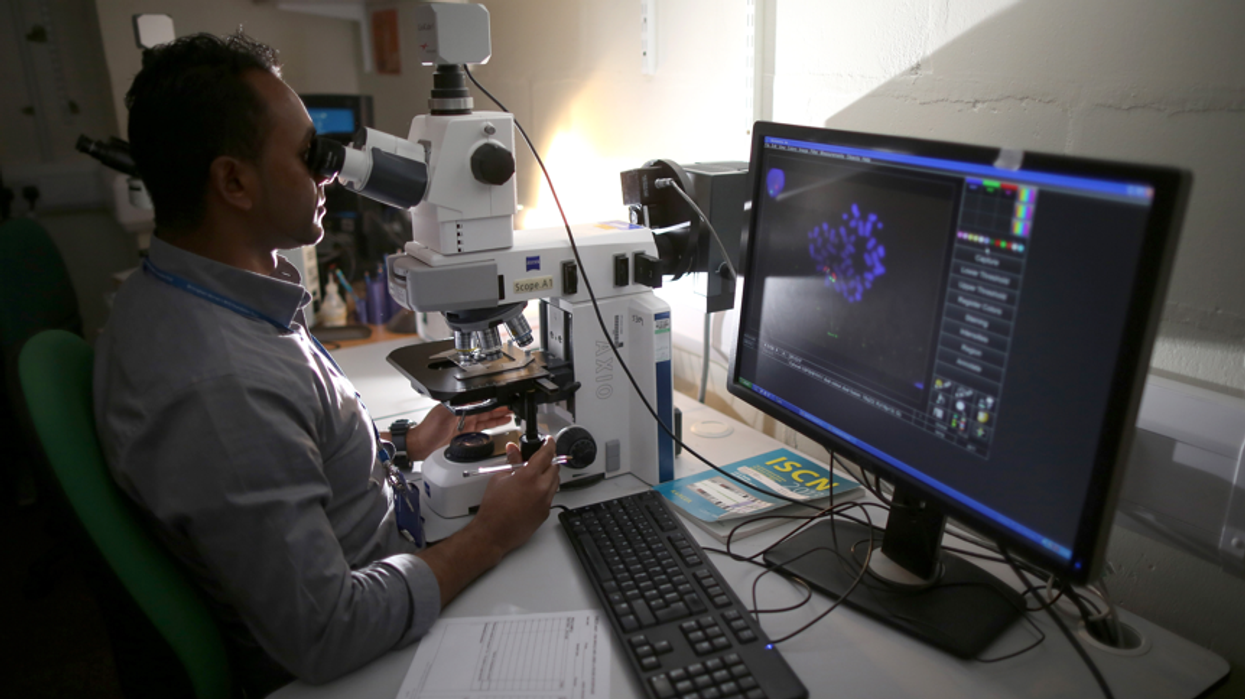
The new system will collect information on a patient’s physical, mental and sexual health held by GP surgeries in England over the past 10 years for a central database.
The scheme, due to start in July, was delayed until September over fears from doctors’ groups that it was being pushed through too quickly.
NHS Digital said during the Covid pandemic, data from GPs helped to identify the most vulnerable people, roll out the vaccine programme and determine hospital treatments which helped prevent further deaths from the disease.
It said the new system will also help plan health services to tackle the long-term impact of coronavirus.
Critics, however, raised concerns that third parties – including researchers at universities, charities or private firms – will be able to access the data.
Kiran Kaur Manku, a neuroscience, ethics and society researcher at the University of Oxford, said the British Indian community understood and valued data sharing for good policy and practice.
He told Eastern Eye: “Despite supporting the concept, due to the lack of information and transparency, much of the community feel mistrust towards the government project. We welcome the delayed deadline for the government NHS data sharing plan.
“However, we call for inclusive actualisation of informed consent and transparency at the data sharing level.
“Much of the British Indian community feel the data sharing plan was not explained to them, and are unaware of the important choice to be made. There are not enough resources to explain the decision to members of the community who are disabled, those not fluent in English, and those excluded in the digital divide.”
Patients can opt out before the data transfer begins next Wednesday (1) by filling in a “Type 1 opt-out” form and sending it to their GP surgery.
They can still opt out of future information being shared after September, but data from the past 10 years may have already been taken from their medical records.
Manku, co-founder of research group The 1928 Institute, added: “In addition to a nuanced informative campaign, we urge the government to be transparent in their decision-making. For example, will an independent ethics committee be making data sharing decisions on a case-by-case basis or will there be blanket rules? Will the independent committee include ethicists, healthcare stakeholders, and lay community members?”

Professor Kamlesh Khunti, professor of primary care diabetes and vascular medicine at the University of Leicester, was among over 200 people from the medical and social research profession who backed NHS Digital’s data sharing plans in June.
He told Eastern Eye: “My view is that it is important for individuals to give access to data as we have seen the power of UK data during the pandemic.
“However, it is important that patients are well informed about what data is being collected, shared and for what purpose.
“Overall, if done properly, data sharing will help management of patients within
health and social care as currently, a number of these organisations cannot access this data to deliver care.”
The move is part of a wider drive to digitise the NHS, including allowing people to access their medical information, procedures and care plans, manage appointments and order repeat prescriptions via mobile phone apps.
Dr Farah Jameel, the British Medical Association’s GP committee executive team lead for IT, believes that when used effectively, ethically and legally, data can play a pivotal role in improving the nation’s health through planning, research or for direct patient care.
She said: “When patients interact with the NHS, they expect that the right staff have access to the necessary information about them, so they get the treatment they need, regardless of whether this is at their GP practice, in a hospital or elsewhere.
“When this doesn’t happen, it’s frustrating for both patients and clinicians. The situation we have at present needs improving, to facilitate better data-sharing between settings.
“Everyone has a right to know what is happening with their healthcare data, what is being shared for wider purposes than just their own care, and who has access to it – as well as to have the final say on whether to share it or not.
“We have seen in recent weeks with the pausing of the GP Data for Planning and Research programme roll-out, what happens when these issues are not communicated properly, and patients are not given an opportunity to take part in such important discussions.”
The social care sector has also asked NHS chiefs to ensure they are included as equal partners in the collection and analysis of patients’ data.
Nadra Ahmed, chairwoman of the National Care Association, said: “There has been an increased focus on the use of data over the past year, which has put increased pressure on care providers to input and keep up to date.
“While we understand the importance of data collection, it is critical that providers are clear about the context of how the data is to be used to improve and support the people we care for in social care.
“Providers must be given the tools to collate and submit meaningful data as requested, as these tasks will be in addition to our primary responsibility, which is to care for vulnerable people across the nation.
“It is also critical that we must not duplicate data collection as providers are currently expected to collate and submit data for several purposes”.
Gurch Randhawa, professor of diversity and public health at the University of Bedfordshire, said informed consent was important to maintain trust between the NHS and patients.
He added: “As health service researchers, we are always open and transparent as to how any data we collect from patients will be used and reported upon, and we provide this information to patients and seek their consent prior to data collection.
“It is important that these principles are also adhered to when introducing the General Practice Data for Planning and Research programme.”
In June, then health secretary Matt Hancock said the move would revolutionise patient care and insisted “data saves lives”. He added: “We have got to get healthcare and how the NHS communicates into the 21st century.”