by LAUREN CODLING
AN NHS leader has urged the public to seek medical attention if they need it, as experts warn delays in getting treatment due to Covid-19 could lead to a long-term risk to people’s health.
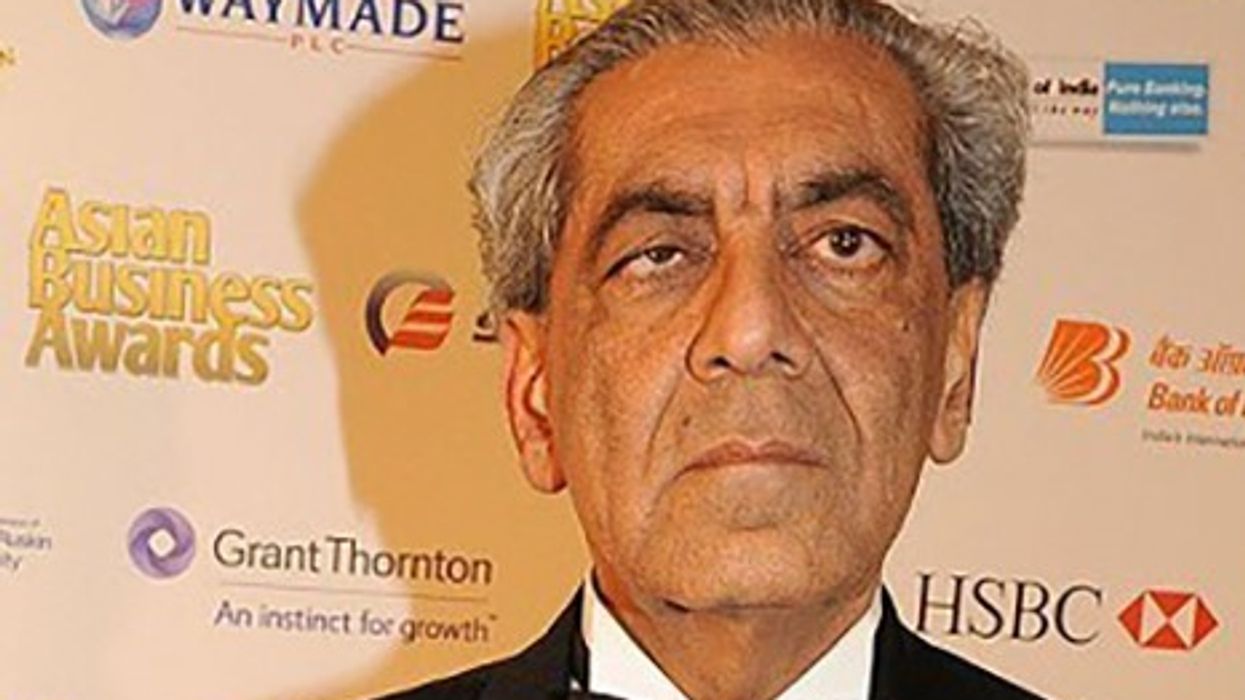
Dr Nikita Kanani is one of several medical professionals who are backing the Help Us Help You campaign, after new figures showed four in 10 people are too concerned about “being a burden on the NHS” to seek help from their GP.
Dr Kanani, the NHS director of primary care and a practising GP, admitted she had noticed patients were reluctant to ask for help, in light of the coronavirus pandemic. “In my own GP practice and across the country, we have noticed that people who don’t have coronavirus – but have other symptoms of illness – aren’t coming and asking for help,” she told Eastern Eye. “Ignoring some of the issues can have quite serious consequences, which you might not know about until the future; so we are urging people to ask for medical help if they need it.”
According to NHS England, in March there was a 29 per cent year-on-year drop in A&E use. Data also pointed out a 50 per cent drop in heart attack attendances. Many other patients have been reported to be reluctant to attend diabetes reviews or maternity appointments due to coronavirus fears.
If people have urgent care needs, they should contact their GP or the 111 service, Dr Kanani advised. If there is an emergency, they should contact 999 or attend hospital if they are advised to.
She is also keen to reassure the public that a lot of healthcare can be done remotely. “It is important to get in touch,” she stressed. “Delaying it is really dangerous and can pose a long-term risk to people’s health."
Dr Kanani admitted there is a possibility that doctors may see an increase of medical conditions following a lift of lockdown measures, including a rise in mental health problems. This could be down to people not contacting their GP and symptoms worsening, but some symptoms may also be triggered by the circumstances of the crisis.
“As people have been indoors, and possibly alone, for a long period of time, they may become more anxious or depressed,” she explained. “We are very aware there will be a change in the health seeking behaviour of the population and we need to make sure that our services are able to look after people as they come through lockdown.”
During the pandemic, most GPs have had to use technology to speak with patients. There has been an increase in remote and online interactions, and the majority of practices now offer remote triage.
Dr Kanani, who works as a GP in south east London, said the switch to digital resources has been a “powerful tool” to ensure patients and staff feel safe. “I would like to congratulate primary care staff who have been working in a very difficult time to innovate and design and deliver care in a different way,” she said.
Looking to the future, she believes people may still want to access care in different ways related to technology. Contacting a medical practitioner via a remote assessment, for instance, could continue to occur after lockdown measures have eased. “I think some of (these practices are) definitely here to stay,” she said.
Since the crisis began, ethnic minority communities have been hit hard by the coronavirus infection. According to findings last week, the death rate of BAME patients with Covid-19 is more than twice that of whites.
On the issue, Dr Kanani admitted BAME workers in the NHS “understandably have real concerns and anxieties about safety (and) about the safety of their families”.
Dr Kanani has urged healthcare employers to undertake risk assessments and explicitly include ethnicity within that, to understand if staff are at risk. “As the evidence emerges, we will continue to work across the system to make sure that our healthcare workers have the support and the protection that they need while they deliver their care,” she said.
















 Crispello was originally launched by Cadbury in the UK in 2012B&M
Crispello was originally launched by Cadbury in the UK in 2012B&M 