MORE EDUCATION AND AWARENESS IS NEEDED TO PREVENT GLOBAL RISE IN RATES OF ILLNESS
CANCER is a challenge for us all. And now, more than ever before, tackling the disease has become a global public health issue as more people live longer.
Cancer rates among Asian people, both in the UK and in Asia, are partly explained by differences in life expectancy and other factors such as smoking, obesity and infection rates. At the moment, cancer rates are lower in countries like India, compared to western economies like the UK, and the most common types of cancer people develop also differ. But as emerging economies undergo radical social and economic changes, their lifestyles become more westernised and we expect to see an increase in cancer rates.
The greatest impact on the number of people diagnosed with cancer in the years to come will be ageing populations. Cancer is primarily a disease of older people, so as more people live longer, more people will get cancer.
In the UK, the number of cancer cases is expected to rise from more than 352,000 a year in 2014 up to 515,000 by 2035.
But while we can’t do anything about age, we can do something to reduce the risk of cancer. Thanks to a landmark study led by Cancer Research UK scientists, we know that around four in 10 cancer cases in the UK can be prevented.
These latest UK figures don’t have an automatic parallel with other countries, because of lifestyle differences among different populations, but they can offer a glimpse at what may be to come for countries undergoing transitions. According to the World Health Organization (WHO), the four most common cancer types in east and central Asia are those of the lungs, stomach, breast and liver.
This is likely to be a reflection of tobacco use and infections in these countries.
Tobacco is still by far the biggest preventable cause of cancer worldwide. But the good news is that the latest UK data points to how tobacco use can be tackled successfully. Over recent decades, smoking rates in the UK have fallen considerably because of strong political action like the ban on smoking indoors and increased public awareness about the harms of tobacco. So, alongside the fall in the number of smokers, we’ve also seen the proportion of cancer cases caused by smoking in the UK fall in the last five years. There’s still more to do though, and as part of the International Tobacco Control Programme we’re committed to helping tackle tobacco worldwide.
It is critical that current increases in smoking rates in Asia are stalled, or ideally reversed, if we are not to see a tsunami of smoking-caused cancers in the decades ahead. In India, we also need to address the high prevalence of chewing tobacco, and in parts of China, high lung cancer rates among women are related to indoor use of smoking fuels for cooking.
You can’t catch cancer, but certain infections can increase the chances of developing the disease. And some of these infections are far more common in Asia, meaning the cancer burden from them is much greater. Most notably are H. pylori, which is a cause of stomach cancer, and Hepatitis B and C, which can cause liver cancer.
Almost three-quarters of new cases of stomach cancer worldwide occur in Asia, and it’s the second most common cancer in the region after lung. In the UK, infections like H.pylori are now less common and as H.pylori infection rates have gone down in Europe generally, stomach cancer rates in the UK have dropped.
While rates of smoking have declined during the last few decades in the UK, and infection rates have stalled, obesity rates have continued to increase. Obesity is now the second biggest preventable cause of cancer in the UK. It’s linked to 13 different types of cancer, including bowel, breast, kidney and oesophageal cancer. Obesity rates in Asia are following the rest of the world, and rising. The WHO recently estimated that nearly half the number of children under five who were overweight or obese in 2016 lived in Asia. This means obesity will have an increasingly greater impact on cancer incidence in Asia in the years to come.
We need more education and information to help people of all ethnicities and backgrounds keep a healthy weight. And we need global political willpower to back up education.
Overall, it isn’t clear whether the picture for Asian people living in the UK is any different from that for Caucasians. However, there are some cancer types where specific cultural factors may be at play; for example, rates of mouth cancer among Asian women in England seem to be higher than white women, possibly because of chewing tobacco such as betel quid or paan.
We also know that uptake of screening programmes – for breast, bowel and cervical cancer – are not as high among Asians in the UK as they should be. Religious and community leaders could help with this by helping Asians overcome any sensitivities or ‘embarrassment’ in taking part.
As the world becomes more adept at tackling infectious diseases such as malaria, TB and HIV/ AIDS, the burden of cancer looms ever larger. It is now the biggest killer worldwide and, if we don’t address some of the risks we know about, this burden will be felt disproportionately in Asia.









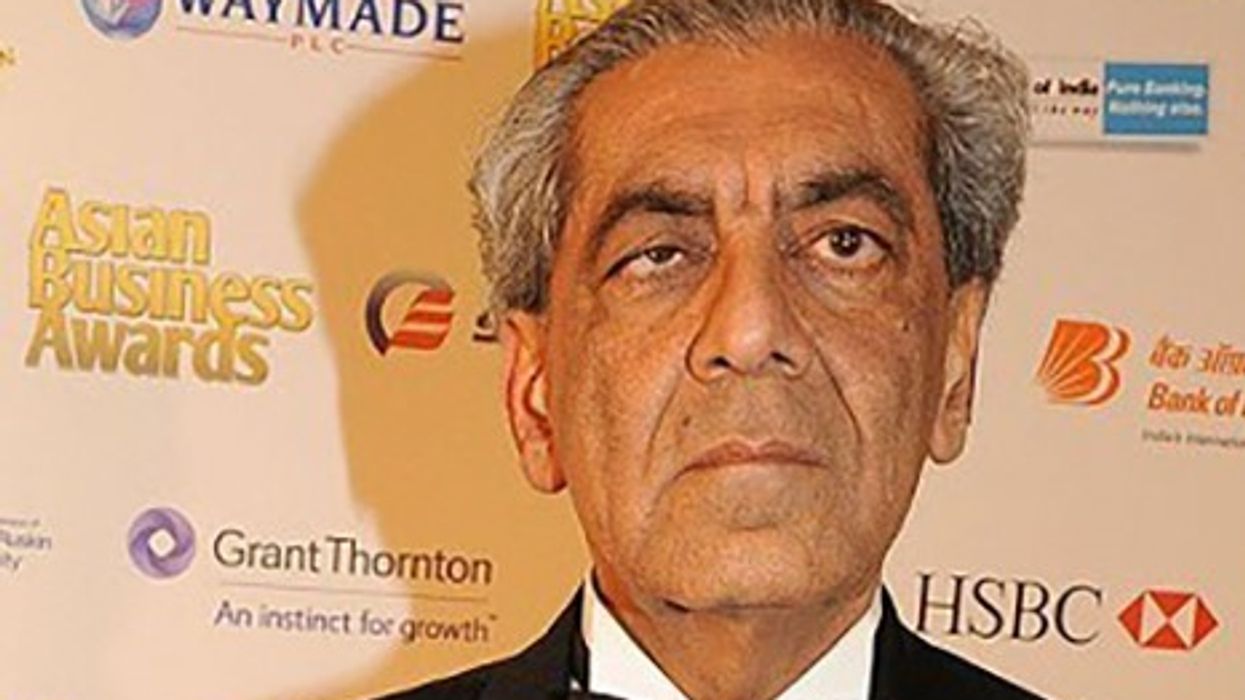











 His Highness Prince Rahim Aga Khan V
His Highness Prince Rahim Aga Khan V
Ending cancer of apathy