BLACK, Asian, and ethnic minority communities are “significantly underrepresented” in precision and genomic medicine research, leading to adverse health outcomes, a study has revealed.
Inadequate ethnic representation in datasets also hinders the development of AI-based risk prediction tools used to estimate the likelihood of diseases or conditions, a report by the University of Nottingham and the NHS Race and Health Observatory said.
The absence of data from ethnic groups “compromises the effectiveness of these tests” across different ethnic populations, the study released last Wednesday (5) said. Precision medicine uses datasets, such as individuals’ genomes or complete electronic health records, to customise medical care.
Genomics can help identify the causes of undiagnosed rare diseases, which helps families avoid prolonged hospital visits and unnecessary tests.
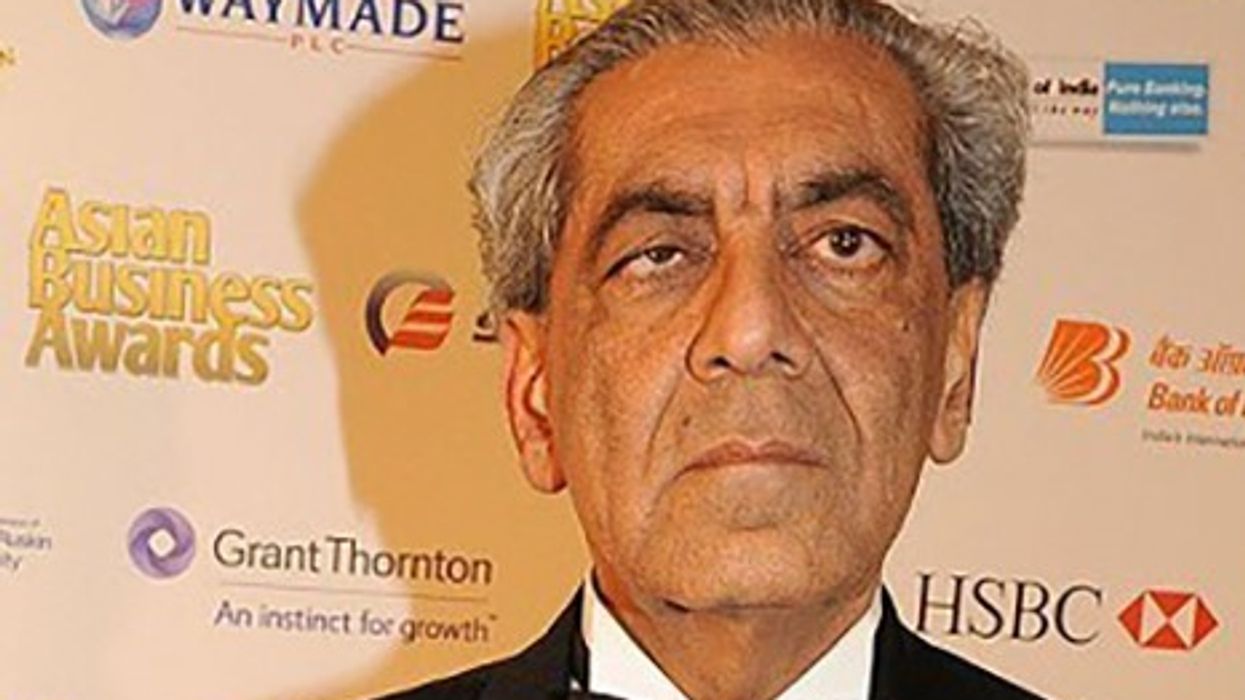
At the launch of the report, professor Habib Naqvi, chief executive, NHS Race and Health Observatory, called for intervention to address minority under-representation in research.
“Genomics and precision medicine are currently at the cutting edge of medical technology and promise a world in which treatments can be more targeted and effective,” he said.
“There is a risk, however, that these advances could leave behind those communities who already experience health inequalities. We know ethnic minorities are underrepresented in medical research and in genomic biobanks,” Naqvi added.
The review of ethnic inequities in genomics and precision medicine looked at 70 policy and guidance documents, from 2017 and 2022. It pointed out that well-documented historical abuses of minority groups by medical institutions led to a loss of trust in research, clinical trial participation, and vaccine uptake.

Researchers said people from minority communities avoided taking part in research due to past violations against them, while others failed to understand how or why their involvement in genetic research could benefit their families, communities, and others.
British Pakistani Sadia Haqnawaz, who lost her baby daughter in 2010 to genetic disorder Autosomal Recessive Polycystic Kidney Disease (ARPKD), said, “For me, It is vital that parents whose babies receive poor diagnoses due to genetic anomalies resulting from consanguineous marriages understand the risk factors involved. Potential, tragic consequences can be avoided if more parents are aware of genetic testing and public health information is available, translatable and accessible to communities.”
“Despite the stigma, cultural, and religious taboos, this is a subject that needs to be addressed and countered against a lot of misinformation around what genetic testing entails from genetic modifications and micro-chipping. Often there is more faith in god than genetic testing and science,” said Haqnawaz, who now works supporting and raising awareness of the risks involved with inter marriages within families.
The review made some key recommendations – such as engaging various groups, including the public, patients, healthcare workers, government officials, as well as authorities in discussions about genetic medicine services; rebuilding trust within communities; ensuring patients and healthcare professionals have access to interpreters proficient in complex medical language; and establishing clear rules and regulations regarding access to genetic data.

“To promote diverse participation in research, there needs to be a change in researchers’ attitudes and behaviours. Research approval groups should mandate the assessment of researchers’ plans for involving ethnic minority communities,” the report said.
“Genetic medicine education should be improved for healthcare professionals. Non-healthcare workers involved in healthcare decision-making, like social workers, chaplains, and community leaders, should receive training on genetic medicine,” the report added.
“Additionally, cultural awareness training should be offered to healthcare workers to enhance patient understanding. Healthcare workers also require specific training to improve the collection of information about a person’s characteristics, including ethnicity.”
Dr Manpreet Bains, the lead author of the report and an associate professor at the University of Nottingham, said precision medicine seeks to deepen our understanding of how differences in genes and other factors impact our health.
“Inequities in access to genomic medicine services are currently evident. It’s crucial to consider the risks to communities experiencing ethnic health disparities. Evaluation and monitoring should be integrated into systems, with clear timelines and measures established from the outset,” she added.
“The report underscored the importance of a diverse workforce, yet inequalities in the treatment of healthcare staff remain a significant issue. Additionally, a lack of understanding and bias among healthcare professionals likely affects clinical practice.”
The report urged collaboration with the National Institute for Clinical Excellence (NICE) to develop healthcare guidelines that consider differences among populations regarding health and disability.
The NHS Race Observatory is currently collaborating with NHS England on an invitation to tender to examine ethnic health disparities within the Genomic Medicine Service.