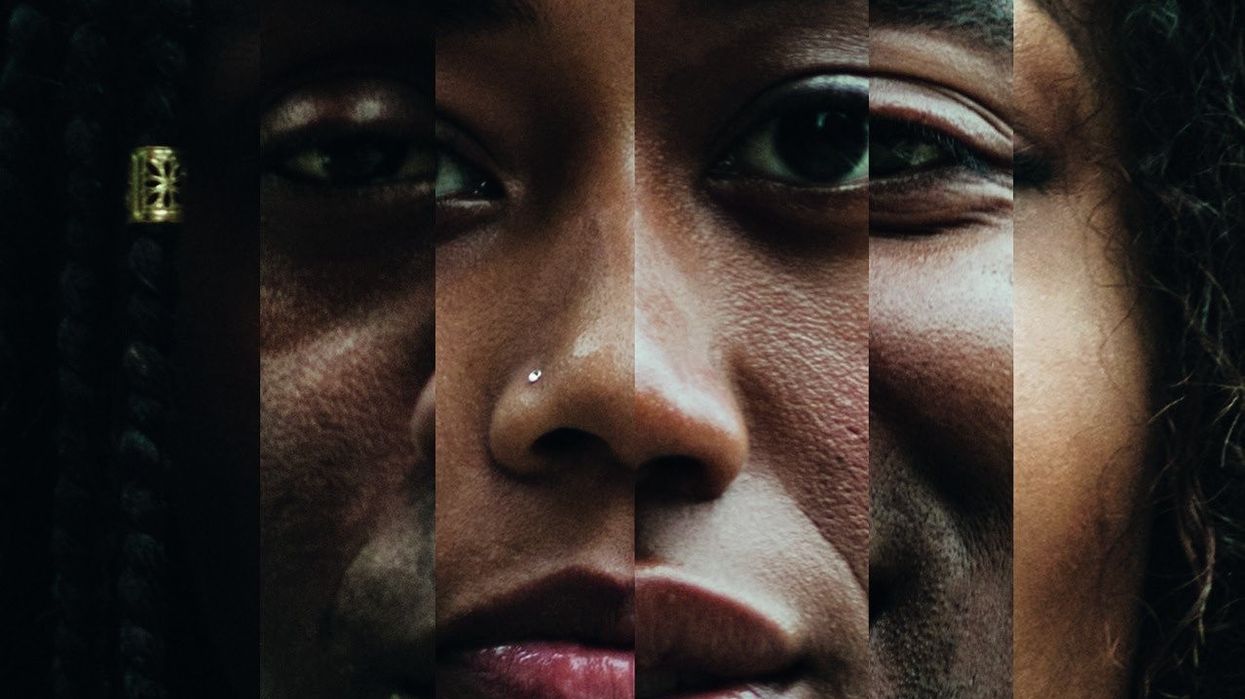
THE Manchester University NHS Foundation Trust (MFT) is set to review and potentially revise its monitoring practices for jaundice in newborns from minority ethnic backgrounds.
This initiative stems from a broader study by the NHS Race and Health Observatory, which highlighted significant disparities in healthcare assessments for black, Asian, and minority ethnic babies.
Around six out of every ten newborns develop jaundice, with those having darker skin being particularly at higher risk.
According to a statement on Monday (22), the MFT announced that it is conducting a review of recommendations regarding the use of transcutaneous bilirubin (TCB) monitoring devices.
These devices are utilised in the screening process to diagnose jaundice, a prevalent condition among newborns. The review will examine the benefits, limitations, and implications of TCB monitoring to ensure optimal care for affected infants.
Dr Ngozi Edi-Osagie, consultant neonatologist, group associate medical director at MFT and principal investigator for the study, said, “We are delighted to be partnering with the NHS Race and Health Observatory on this vital piece of work which will provide further insights into the effective and timely diagnosis of jaundice in newborn babies with darker skin in the community, which will lead to improved clinical outcomes.”
The 12-month review will survey existing studies, products, and assessments used in paediatric care, and analyse jaundice incidences in ethnic minority newborns compared to other groups, involving input from local communities.
To gain further insights, the Caribbean and African Health Network (CAHN) will spearhead surveys and structured interviews with mothers, service users, and families from the broader community. The study, led by Saint Mary’s Managed Clinical Service of MFT, will collaborate with experts from the University of Central Lancashire, Imperial College London, and CAHN.
Prof Habib Naqvi, chief executive of the NHS Race and Health Observatory, said, “The colour of someone’s skin or their ethnicity should not impact health outcomes, and yet we know, from data and evidence, how too many avoidable inequalities remain persistent for our communities.
“We have a duty to take immediate action on de-biasing current clinical guidelines, assessments and practices, and to prepare the next generation of healthcare professionals in ensuring fair health outcomes for all groups in society.
“That’s why we are pleased to commission this work, which seeks to ensure early, accurate diagnoses and treatments to help prevent serious and avoidable complications resulting from jaundice.”
The study will also evaluate the accuracy of TCB monitors in diagnosing jaundice in babies with different skin tones, compared to traditional subjective assessments.
Practical recommendations for clinical practice, including guidance for healthcare providers and families, will be identified. The initiative will consider the cost and implications of TCB monitoring on clinical practice, particularly regarding the late diagnosis and treatment of jaundice.
The study follows last year’s Observatory commissioned report, led by Sheffield Hallam University, which identified a several limitations around current neonatal assessments and perinatal practices.