NEW guidance encouraging GPs to focus on the wellbeing of themselves and their staff will be difficult to follow due to mounting workloads and more needs to be done, according to experts.
The British Medical Association union has urged family doctors to rotate workers between high and low stress activities, be alert to signs that colleagues might be in need of help and ensuring that senior staff are visible and available to talk.
It also advised GPs to arrange support groups and safe spaces for staff to speak openly, make them aware of the support available and encourage them to take breaks.
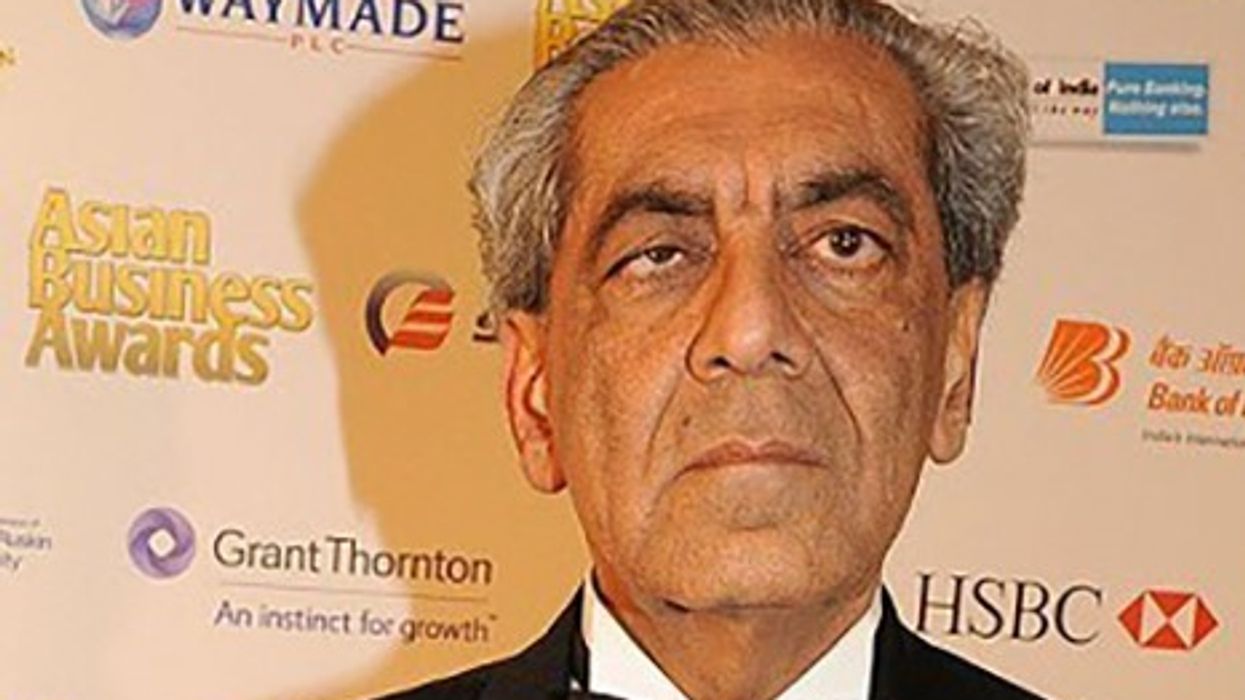
Dr Ajay Gupta, from the centre for clinical pharmacology and precision medicine at Queen Mary University of London, told Eastern Eye: “The BMA’s guidance – including increased visibility of the senior staff, provision of support and safe spaces to staff and ensuring a system of peer support – are all good practices that have been shown to improve emotional well-being and reduce burn-out among healthcare professionals.
“However, whether GPs have the time, resources or training to implement these changes is another catch-22 situation. “More out-of-box thinking is required to change the system, instead of recycling this advice and trying to optimise a system when the latter is working beyond its capacity in the first place.”
With GPs under pressure, the government in May announced that pharmacists will be able to give out prescription medicines and oral contraception to patients without GPs’ sign-off.
Treatments for seven common conditions – including earache, sore throat and urinary tract infections – are expected to be available in chemists without seeing a doctor from this winter.
Prime minister Rishi Sunak said he hoped the measures will help end the “alltoo stressful wait” for appointments by freeing up 15 million slots at doctors’ surgeries over the next two years.
Dr Chris Papadopoulos, principal lecturer in public health at the University of Bedfordshire, told Eastern Eye: “The publication of this guidance is a positive step towards acknowledging and attempting to support GP mental health which we know from the research evidence is poor.
“This isn’t surprising given the increasing levels of burnout and poor morale currently present in the workforce.
“However, the reality is that issuing guidance on how GPs can support their mental health simply is not enough.
“Most GPs will already have knowledge of such measures, but won’t have had the time or energy to act upon them.
“What GPs really need is better work-life balance, compassionate and safe workplace environments and access to supportive services and professional support - this costs money, but will likely be more effective than issuing them more guidance that GPs may perceive as more demands on them.”
Dr Judith Johnson is an associate professor in psychology at the University of Leeds and an expert in psychological resilience. She said: “Most of the suggestions don’t actually require more time, but they do require careful consideration.
“For example – encouraging a kind workplace, where colleagues look out for each other, requires a whole organisational shift.
“Management needs to be invested and to model this behaviour for their employees, as well as then creating opportunities for this to occur; for example, through coffee breaks and rewarding it.
“Rewards can be ‘soft’ such as verbal praise or ‘hard’, for example, by building it into appraisals. So, while this is just a bullet point on a list, the reality of implementation is quite different.”
Research in May found that 54 per cent of doctors admitted the impact of staff shortages on patient safety is affecting their own mental health.
A survey by Medical Protection, which represents more than 300,000 healthcare professionals around the world, found that two in five medics feared being sued or investigated due to incidents arising from staff shortages and that had a detrimental impact on their wellbeing.
Among those surveyed, 49 per cent acknowledged they are considering their career in medicine due to the impact of staff shortages on patient safety.
Medical Protection president, Professor Dame Jane Dacre, said: “The fact that most doctors feel the under resourced environments they work in presents a significant threat to patient safety, is a sad reflection of the times and is distressing for patients and doctors alike.
“The effect of not being able to provide excellent or even adequate care on a doc[1]tor’s mental wellbeing cannot be overstated. Nearly half the doctors we surveyed said they are considering their career in medicine because of this.
“The workforce is exhausted, fearful and many need support with mental health issues. When doctors’ mental wellbeing is poor, it is not only damaging for them, but also jeopardises patient care.”
The UK government recently announced that it had met its manifesto pledge of recruiting 26,000 additional primary care professionals such as dieticians, paramedics and physiotherapists to support doctors and nurses.
There are now 29,103 additional primary care staff and since March 2019, there are three and a half times more people working in these roles in GP practices.






 JD Vance and family step off the plane in traditional attire receiving a warm receptionTwitter Screengrab/PTI
JD Vance and family step off the plane in traditional attire receiving a warm receptionTwitter Screengrab/PTI