INDIA’s government grapples with the Covid-19 outbreak that threatens to become the world’s most severe, reports The Times.
India is the third-worst-hit country for Covid-19 cases, and catching up quickly with the US and Brazil in first and second place. Over 50,000 Indians have died since the outbreak began — the world’s fourth-highest total — with more than 2.5 million infected.
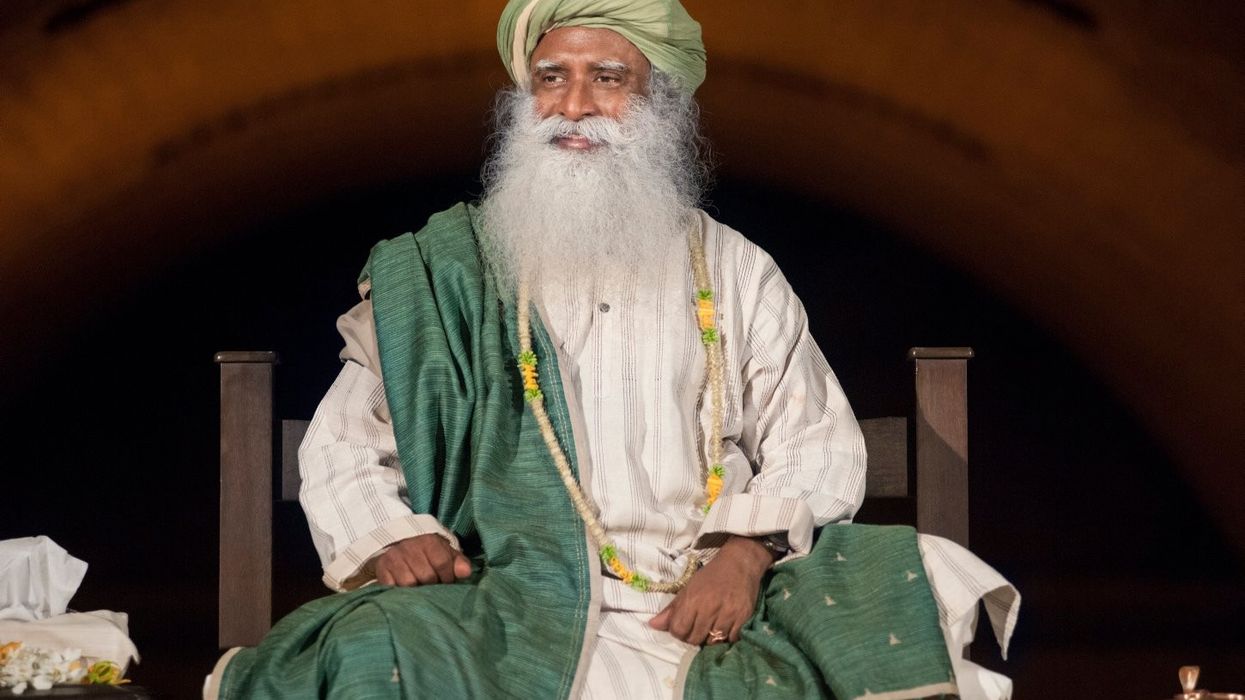
Last week, the country saw a record one-day rise of 67,000 new cases. Among them was an octogenarian holy man Mahant Nritya Gopal Das, who had sat on the dais with Modi during the Ayodhya temple ceremony.
“I’m very worried about where India goes from here. The trend line is only going up. I would not be surprised if India overtakes Brazil soon, and at some point moves past the US too," said professor Ashish Jha, the Indian-born director of the Global Health Institute at Harvard.
“India’s investment in primary healthcare is abysmally low especially in places such as the rural state of Bihar. When I speak to my cousins back home, it is clear no one is prepared for what is coming.”
India declared a harsh nationwide lockdown in March. Once the lockdown was lifted, a second crisis hit, as millions of poorer migrants fled cities such as Mumbai and Delhi and returned to villages in the hardscrabble heartlands. Now, the disease takes hold in its poorer interior, The Times report said.
Numbers are rising in places such as Uttar Pradesh — a state that on its own has a population larger than Brazil’s, but often lacks even the basic hospital facilities found in India’s largest cities.
A recent study pointed out that more than half of residents in three Mumbai slums had tested positive indicating that government statistics were undercounting the outbreak’s severity.
“Our study suggests the actual spread may be way, way more than we thought, and thus the death rate is also lower than the official figures, which is good news,” said Reuben Abraham, of the IDFC Institute, which co-authored the research.
According to the news report, bureaucrats failed to use the breathing room provided by early lockdowns to build up hospital capacity outside the main cities, invest in personal protective equipment for medical staff, or build a rapid national contact tracing system.