THE defence lawyer has condemned his own client, the father of murdered 10-year-old Sara Sharif, saying he would suffer "in the circles of hell for eternity" for his crimes against his daughter.
The statement came during closing arguments in the trial of Urfan Sharif, 42, who stands accused alongside his wife Beinash Batool, 30, and Sara's uncle Faisal Malik, 29, for the brutal murder of Sara at their Woking home in August last year. They all denied the charges.
Defence barrister Naaem Mian KC has branded his own client "a scumbag" while attempting to navigate the complex web of responsibility surrounding Sara's death. "What happened to Sara was awful, and that must be the understatement of the year. It was savage, it was brutal," Mian told the jury.
During the trial Urfan, a taxi driver, reversed his initial defence strategy of blaming his wife. On the seventh day of giving evidence, he made an admission of "full responsibility" for Sara's death, confessing to beating her with a cricket bat and metal pole - though he maintains he never intended to cause serious harm.
The court heard horrific details of Sara's injuries, which included dozens of broken bones, human bite marks, and burns from both a hot iron and boiling water. Part of her finger had been cut off with a sharp instrument, and evidence suggested she had been hooded during the abuse.
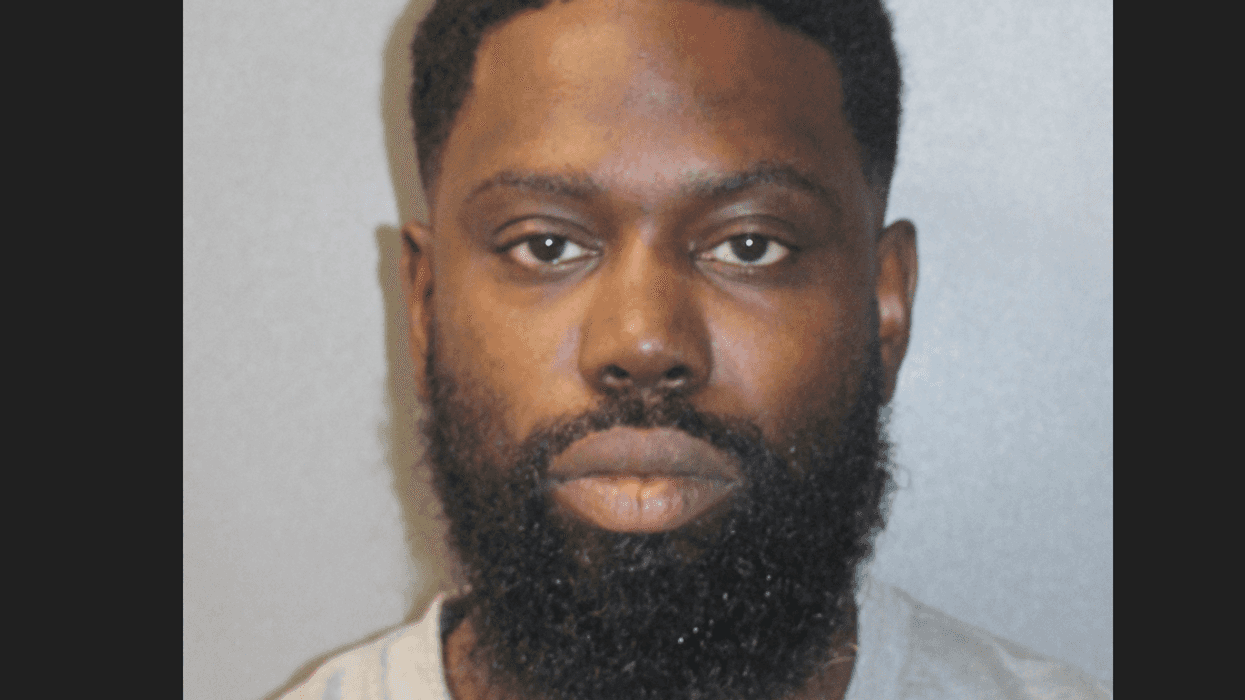
Urfan Sharif, Beinash Batool and Faisal Malik. (Photo credit: Surrey Police)Despite these admissions, Urfan's lawyer attempted to create doubt about the final moments of Sara's life. He pointed out that only Batool was present when Sara died, telling jurors, "The only person who can say what happened on the Saturday, Sunday, Monday and Tuesday when Sara is in her arms is her."
The mystery deepened with evidence that Batool made 30 calls to family members instead of contacting emergency services when she realised something was wrong with Sara. The day before Sara's body was discovered, all three defendants fled to Pakistan, only returning later to face charges.
Batool's lawyer, Caroline Carberry KC, forcefully rejected the attempt to shift blame onto her client, describing Sharif as the only "psychopath in the courtroom" and a "comfortable liar".
She highlighted Sara's spirit, quoting teachers who remembered her as "spirited, bold and fierce", suggesting that these very qualities might have triggered Sharif's violent responses.
The prosecution painted a picture of a household where violence had become normalised.
Police found damning evidence including a bloodstained cricket bat and a rolling pin bearing Sara's DNA in the family's outhouse. Prosecutor Bill Emlyn Jones KC argued it was "inconceivable" that any one defendant could have carried out the abuse without the knowledge and complicity of the others.
The case has also raised serious questions about the role of social services and the family courts system. Sharif's own lawyer suggested these institutions shared some responsibility, noting they were aware of previous accusations against his client yet still allowed him to gain custody of Sara.
As the trial draws to a close, the jury must now grapple with multiple charges against each defendant. All three have pleaded not guilty to murder, causing or allowing the death of a child, and the alternative charge of manslaughter.
The prosecutor reminded the jury of their duty: "If you know it is happening you do something to prevent it. None of them did because they were, and are, all responsible for her death and they all are guilty of her murder."
The trial at the Old Bailey continues, with the jury expected to begin deliberations soon.