Racial justice is essential in all democracies and progressive societies, which seek to learn from historical examples of persecution, incarceration, and enslavement on the basis of race.
Anti-slavery and civil rights movements in the North America and Europe led to greater freedoms, alongside campaigns to tackle gender disadvantage and discrimination.
Healthcare is a product of generations of societal and institutional policies and wider sentiments in society which evolve with time.
History also shows many examples of scientific racism and the use of medical power and authority as an agent of the state. This is a worrisome possibility against which health professionals, professional regulators, charities, and membership societies battle.
Therefore, although it may be difficult to accept, racism is evident in medical and nursing training, in the current delivery of care, in knowledge production and research, and the formulation of our laws and policies and in NHS care.
The NHS leadership recently committed to an anti-racist strategic plan for medicine. Much is being done to tackle racism in these arenas, especially since we lived through COVID-19 and Black Lives Matter, dystopian reminders of how poorly we have understood or dismantled structural drives of inequalities, health inequalities, and racism specifically.
Yet racism and discrimination more generally are common, with up to a third of people in population survey accepting they discriminate against other on grounds of protected characteristics. There is often silence when racism is felt, or reported, so there is little research on how it manifests, and what we can do about it. Many public institutions repeatedly fail to put in placed sustained actions that accept and respond to racism, including police, education, criminal justice and in employing organisations. Furthermore, racism mostly affects those at the intersections of multiple disadvantages, and they are the most vulnerable to its pernicious effects on health.
Racism comes in many forms and is associated with poor physical and mental health, as well as social, financial, education, and societal consequence including likelihood of entanglement in the criminal justice system.
Racism in mental health care has been topical precisely because attempts to explain the racial and ethnic disparities in the incidence of mental health problems, psychosis specifically, and because racial and ethnic minorities are more likely to receive coercive care, for example, by detention and forced treatment under the powers of legislation (the mental health act), and less access to appropriate psychological and social therapies.
Given decades of data showing racial and ethnic disparities in mental health care, it is surprising little has shifted, in part as the structural drivers of racism have not been understood to taken seriously.
Talking about racism and responding to is not easy. Racism is experienced as thorny and sensitive topic; people fear offending each other and that their vocabularies and lived experiences are not conducive to empathising or understanding what it is like to be on the receiving end of racism. They fear racist attitudes and behaviours might be exposed and condemned, and they will be vilified.
Our new paper (from Oxford, QMUL and Birmingham and published in the British Medical Journal Mental Health, funded by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration – North Thames) looked at in-depth interviews with 10 people and identified some explanations for why and how racism persists on inpatient mental health. We used novel methods that are fully explained in the paper.
For methods experts and critics, we undertook secondary analysis of experience data, collected through qualitative interviews, and we applied critical realist methods to better understand how contexts trigger particular mechanisms, to produce particular outcomes in those contexts. Therefore, we expose common mechanisms by which racism is generated and persists. These should be the focus of future intervention and evaluation against health, social, and quality of life outcomes for patients and staff working in these challenging environments.
Our paper shows how racism manifests and persists on inpatient mental health units through the following mechanisms:
- An absence of safe spaces to discuss racialisation which silenced and isolated patients
- Strained communication and power imbalances produced mutual racialisation by patients and staff.
- Non-reporting of racialisation and discrimination, which led to feeling othered, misunderstood, disempowered and fearful.
- Furthermore, persistent racialisation prevented authentic feedback and staff-patient rapport and the opportunity to help recovery and respond to patients’ concerns.
- Racialisation went both ways, between staff and patients, contributing to a toxic and unhealthy environment for both, given we know experiencing racism is bad for your health.
The findings are surprising given the emphasis in professional training and public institutions to stamp out discrimination. Therefore, people already in distress, and who may be detained or living on the inpatient unit voluntarily to receive care, are met with further traumatic experiences that hinder recovery. Our paper clearly shows opportunities for creating safer environments in which people who are suffering mental illness and are detained.
Racism is a public health problem given it is common and is known to affect health and wellbeing through interpersonal, institutional and structural manifestations. However, whenever there is an attempt to acknowledge and respond to racism, history shows many examples of resistance to such ideas. This comes in many forms: denial, personal objection and counter-claims of being vilified and ill-treated, government proclamations as well as institutional assertions of equity and fair principles in public institutions.
Changing the way racism is dealt with may help improve safety and recovery more generally, but policy makers, commissioners, managers and practitioners must commit to dismantle cultures of silence, improve training and skills in cultural capability, ensure reporting processes are known and taken seriously with visible actions. Particularly sad is people on inpatient mental health units are admitted in order to protect and promote their mental health, not to compound it, especially if they are there under the powers of the Mental Health Act, when they cannot leave.
CHiMES manifesto of proposed actions:
- ‘You said – we did’ statements on racism on inpatient mental health units and throughout health and social care.
- Detailed experiential, co-designed, participatory research to understanding how to support practitioners, and patients encountering racism.
- All health, social care, and public policies need to be tested for equalities impacts, including race equality.
- Development and implementation of co-designed experience driven systems interventions.
- NHS Leadership Teams must put in place trauma-informed systems for reporting and responding to racism, discrimination, and gathering authentic experience data to improve safety and quality
- Recruitment, training, and retention of staff needs to better recognise the knowledge, skills and attitudes required to combat racism in inpatient and community care, especially for those facing coercive care.
- Public health actions, including curricula in schools, universities and apprenticeships, must embed the conceptual tools and skills to talk about and address injustice and inequity in society, including racism and mental health.
Prof. Kam Bhui CBE MD FRCPsych
CHiMES collaborative, University of Oxford.
Building interdisciplinary, creative, lived experience coalitions to protect and promote equity and mental health across the life course.












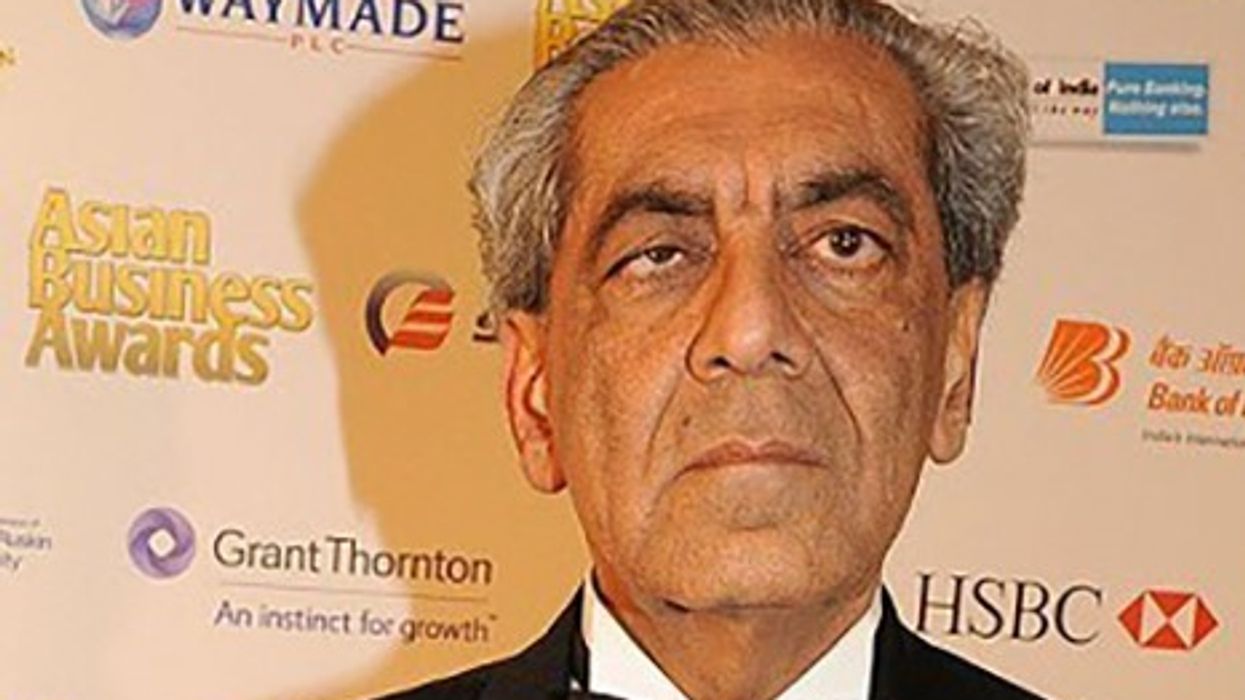





 His Highness Prince Rahim Aga Khan V
His Highness Prince Rahim Aga Khan V


Talking about and tackling racism in mental health care