The Mind mental health charity said mainstream services often fail to provide therapies that meet a person’s cultural or language needs and they are not referred to the right support.
It comes after a study in May by the Mental Health Foundation found that people from a black, Asian or minority ethnic background are at a higher risk of reporting loneliness than other groups. Overall, a quarter of people have felt lonely some, or all, of the time over the previous month.
Marcel Vige, head of equality improvement at Mind, called for urgent further investment for support services that are close to people’s homes and existing support network. He told Eastern Eye: “The pandemic has had a huge impact on the nation’s mental health, which has widened existing inequalities.
“Awareness campaigns are helping tackle the misunderstanding around mental health and encouraging those of us who are experiencing poor mental health to open up.
“However, there is still mental health stigma attached, this can be particularly true for people from south Asian communities where community norms can be experienced as barriers to people speaking up, also stereotypes about people living in self-supportive communities mean services can be less responsive.”
Vige added: “Even in cases where people do feel able to seek support, mainstream mental health services often fail to provide accessible services that meet the particular cultural or language needs, and too often people are not referred to the right support.
“The UK government must start tackling the social factors which can really impact someone’s mental health such as financial and housing worries, loneliness and isolation, employment, racism, and racial trauma.”
Meanwhile, new research from biography-writing service StoryTerrace found that around one in three people from ethnic minority backgrounds said they have little understanding of their cultural heritage.
And 25 per cent said not knowing enough about their cultural origin negatively affects their wellbeing such as developing feelings of guilt, imposter syndrome or loneliness.

Professor Dinesh Bhugra, professor of mental health and cultural diversity at King’s College London, told Eastern Eye: “People with long-term illnesses may experience stigma against their illness more so if it is mental illness, which may isolate them further.
“The pandemic has led to [less] social contact thereby creating a sense of alienation leading to double jeopardy in many minority groups.”
On the research by StoryTerrace, professor Bhugra added: “Our heritage teaches us language, religion, and other aspects of our identity which makes us who we are.
“Not knowing or knowing certain partial bits can affect an individual’s identity and how they function.
“Identity is critical for all of us because that is how we see ourselves but also (how) we see others seeing us, if we are uncertain about our identity then it is going to affect our functioning.”
Some 76 per cent of British Indians face barriers in accessing mental health care, according to research earlier this year by The 1928 Institute think-tank.
And 86 per cent said they faced discrimination and 81 per cent reported feeling shame or stigma when accessing NHS mental healthcare.
Kiran Kaur Manku, from The 1928 Institute and a professor at the department of psychiatry at the University of Oxford, said: “In our work commissioned by NHS England, we found that 93 per cent of British Indians feel the clinical approach to mental health by the NHS is alienating. Critically, participants called for a multidimensional approach to mental health, which includes values, spiritual
philosophies, and history.

“This urgently needs to be addressed.”
Naushad Qayyum developed symptoms of Post Traumatic Stress Disorder (PTSD) after his father died of a heart attack on his son’s wedding day.
After undergoing therapy and practising regular mental health exercises, he is now a campaigner for suicide awareness.
Qayyum, from Leeds, Yorkshire, said: “What my experience taught me is that we have to talk – especially men.
“Where suicide rates are at the highest they have ever been, we have few options left. “Talking about my experiences with StoryTerrace helped me feel connected to myself, it helped me remember things I thought I had forgotten and allowed me to let go of shame. “Seeing my experience in writing and re-reading what happened is an incredible tool to help me process what happened.”
In May, the government said it is over half way to delivering on its manifesto pledge of having 26,000 more primary care staff by March 2024. This includes mental health practitioners and social prescribing link workers, who refer patients to community services to support their wellbeing.
There are now over 18,200 more people working in general practice in March 2022 compared to March 2019 and nearly 30,000 overall.
Health and social care secretary Sajid Javid said: “I am hugely grateful for the tireless work of GPs and primary care staff who act as the ‘front door’ to the NHS and provide advice and support to their patients.
“We have been working closely with the NHS to continue building the workforce and tackle the Covid backlog. “With over 18,200 more primary care staff already, we are on track to deliver 26,000 more by 2024, backed by record funding to help increase capacity and get patients the care they need more quickly.”
Elsewhere, millions of school pupils now have access to specialist mental health support, NHS England said.
A record 650,000 children and young people were in contact with NHS mental health services over the last year, up from 534,000 before the pandemic.
Mental health support teams are now in place in around 4,700 schools across the country offering support to children with conditions including anxiety and depression. Referrals to the teams can be made by teachers or GPs, or young people can even refer themselves.
Claire Murdoch, head of mental health care in England, said the services will provide a “lifeline for many young people who are struggling and need some help”.
Anyone feeling emotionally distressed can call Samaritans for help on 116 123, email jo@samaritans.org or ring Mind’s information line on 0300 123 3393

















 Damian Talbot
Damian Talbot
 Nirmala Sitharaman speaks at the India-UK Investor Roundtable in London last Wednesday (9). On the panel were India’s department of economic affairs secretary Ajay Seth and Kotak Mahindra Bank founder Uday Kotak
Nirmala Sitharaman speaks at the India-UK Investor Roundtable in London last Wednesday (9). On the panel were India’s department of economic affairs secretary Ajay Seth and Kotak Mahindra Bank founder Uday Kotak Sitharaman with Sir Keir Starmer and Rachel Reeves
Sitharaman with Sir Keir Starmer and Rachel Reeves Sitharaman with Jonathan Reynolds
Sitharaman with Jonathan Reynolds 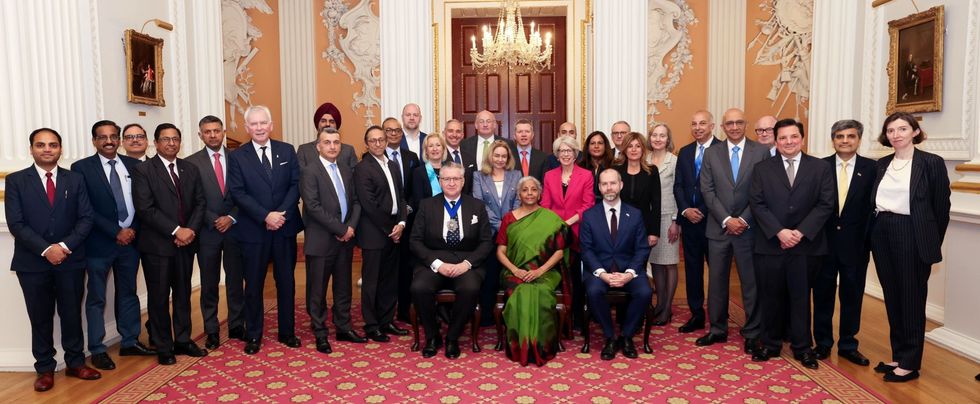 Sitharaman with Reynolds, Alastair King, India’s high commissioner Vikram Doraiswami and other delegates
Sitharaman with Reynolds, Alastair King, India’s high commissioner Vikram Doraiswami and other delegates